People often mistake sympathy for empathy. So what’s the difference? Sympathy is the acknowledgement of the suffering of others; it’s acting as an observer, watching at a distance. Empathy is the ability to fully understand and share the feelings of another; you’re a participant able to experience with the other person.
Put simply — sympathy accommodates; empathy empowers.
Why empathy matters: an anecdote
You may remember hearing about US Airways Flight 1549, or more likely, about its pilot, Sully. On January 15, 2009, soon after takeoff, Flight 1549 struck a flock of geese and lost all engine power. Unable to reach any airport, pilots Sullenberger (Sully) and Skiles decided to attempt a water landing on the Hudson River off Midtown Manhattan. All 155 people aboard survived. The landing was deemed a miracle and Sully hailed as a hero.
That wasn’t the end. 18 months of investigation followed. Some theorized that the pilots could have made it to one of the nearby airports and landed safely on a runway rather than in the Hudson River.
To test the theory, investigators used flight simulators. The simulators showed the plane could have landed safely at a nearby airport. The pilots insisted they wouldn’t have made it. Why the discrepancy? What was the investigative team missing?
They were missing the human truth.
Pilots in the simulations had been prepped. They knew what would happen; they knew the recommended course of action; they could act immediately. The reality for Sully and Skiles was much different. They had to contend with not only the surprise of being struck by birds and needing to assess the severity, but also fear for their own lives and those of the 155 people they had on board. That’s a lot to handle in a matter of seconds.
When you look at that situation without empathy, the answer seems simple. But when you consider the pilots’ emotional states, it instantly becomes complicated. Because humans are complicated. Emotions are messy. And the physical and mental response to stress is unpredictable.
So what does this have to do with healthcare?
Healthcare is personal, and as such, healthcare is stressful. The “happy path” rarely exists in healthcare decisions. We must design for stress.
How do we discover human truths?
If empathy hinges on understanding human truths, how do we discover them? There are multiple ways of getting there.
1. Mindfulness training
Training healthcare professionals in mindfulness can improve their abilities to be present while listening to patients, understand and develop insights on the patient experience, and acknowledge and manage their own stress levels and biases. All of these skills open them up to empathizing more deeply with others.
Research in neuroscience suggests that the insula is an area of the brain that is very important for empathy. Some studies have also shown that people who practice intermediate levels of mindfulness have thicker insula compared to control groups, suggesting that mindfulness training can change the brain and make trainees more empathetic.
Behavioral studies have shown similar results; participants in one study were 3x more likely to give up their seats to a woman on crutches after completing mindfulness training than those who didn’t receive the training.
2. Simulation training
Simulation training is recreating an experience through artificial conditions. It could be using virtual reality (VR), or something more low-tech like using a blindfold to simulate low or no vision. Excedrin recently used VR to simulate the symptoms of a migraine, with the goal of helping non migraine sufferers better understand the severity of the condition. The simulation mimics aspects of a migraine, such as sensitivity to light and sound, disorientation, and aura.
Simulations can be a great way to gain a baseline understanding, but cannot account for the intangibles and unpredictability of living with a condition or experiencing a trauma. In fact, some studies suggest that simulations, specifically those dealing with disabilities, might inhibit empathy.
Simulations should not be used in isolation. In order to truly make them impactful, simulations should be paired with other empathy-building techniques.
3. Ethnographic studies and contextual inquiries
An ethnographic study is the practice of immersing yourself in a subject’s natural environment for a significant period of time. These studies are observational in nature; the researcher is living as part of the group. Contextual inquiries, however, are part ethnographic, part interview, allowing the researcher to observe as well as ask questions about those observations. These inquiries are often conducted with a specific system or process in mind.
Field studies, such as these, are extremely valuable in gaining qualitative insights, uncovering patterns or behaviors that subjects are often unaware of or wouldn’t think to disclose in an interview. These approaches are well suited for understanding complex cultural, societal, and unpredictable situations, as illustrated in Brand Quarterly’s article Why Context Matters: The Power Of Ethnography In Design.
As such, they’re particularly relevant to the patient experience, which is too nuanced and emotional to be fully illustrated with quantitative research like surveys or numerical data. Seeing patients only in the healthcare setting doesn’t allow practitioners to understand their true lifestyles and priorities. Examining people in their own environments, surrounded by people, things, and processes that are familiar and comfortable, helps to paint the broader picture of their human experiences.
The truth lies in what people do when they’re in their element.
4. Empathy interviews
Empathy interviews are a question-and-answer format used to gather qualitative insights. These interviews focus on the emotional and subconscious aspects of an experience and are most effective when conducted in person. They’re all about following the details: tone, speed of speech, body language, facial expression, eye contact, specific word choice.
As with ethnographic and contextual inquiries, empathy interviews are best conducted by an experienced professional. The interviewer must be trained in recognizing the significance of certain microinteractions and nuances in communication, and have the wherewithal to go off script with the situation calls for it. It’s essential not to lead the interviewee. Pay attention and follow where they take you.
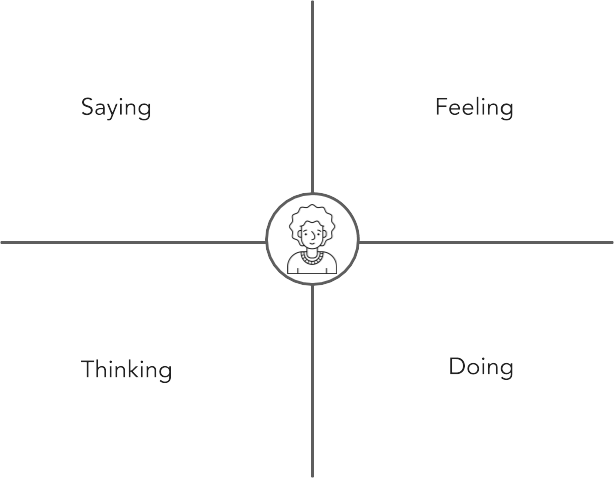
5. Personas and empathy mapping
Persona and empathy mapping is about creating a framework or modeling of the emotional state of a particular audience or persona. By conducting this exercise, you can glean high-level insights, validate decisions, and make technical data or processes more approachable – all while protecting the privacy of patients.
Success comes when empathy goes beyond the research team. Personas and empathy mapping are tools to humanize research. They allow the larger team to digest research findings in ways that are human, empathetic, and easily translatable to design and process decisions. Every idea should be weighed against the applicable personas and empathy maps, and, ultimately, vetted with real patients.
Where does digital fit?
Digital interactions designed without empathy can be a blight on the entire healthcare experience. When someone comes into a doctor’s office with a cough and a runny nose, the doctor knows that it’s 99% likely to be a cold. But that 1% chance that it’s not is what’s likely lurking in the back of the patient’s mind. Ignoring that stress is a mistake, and while doctors are trained to attune to patient concerns, websites are not. A website or email or anything digital is only as empathetic as the humans who create it.
Without empathy at the core, those digital interactions–which can be the first interaction and sometimes the most constant contact a patient has with your brand–can weigh down the healthcare experience. Patients have many choices when it comes to healthcare, and they won’t hesitate to go elsewhere if they don’t get what they need.
To make healthcare more human–that is, to root the experience in empathy–do the following:
- Speak like you care
- Be transparent
- Help people prepare
- Alleviate onus on the patient
- Be proactive, rather than reactive
- Ask for input
- Respect patients’ time
- Instill trust
- Personalize
- Adapt to context
- Be accessible
Empathy is a journey, not a destination
Empathy is not something you can devote a couple weeks to and be done with it. Empathy is a process, and something that should continue beyond the initial strategy or design phases. Digital experiences are shifting constantly, and with them, patient expectations are evolving as well. It’s important to continue to check in with, observe, listen to, and empathize with the people under your care.
For more, watch our recorded HCIC Backstage Pass Webinar on designing for empathy in healthcare.
To speak to one of our healthcare experts about how to create digital patient experiences that are founded in empathy, contact us.